Health Insurance & TPAs
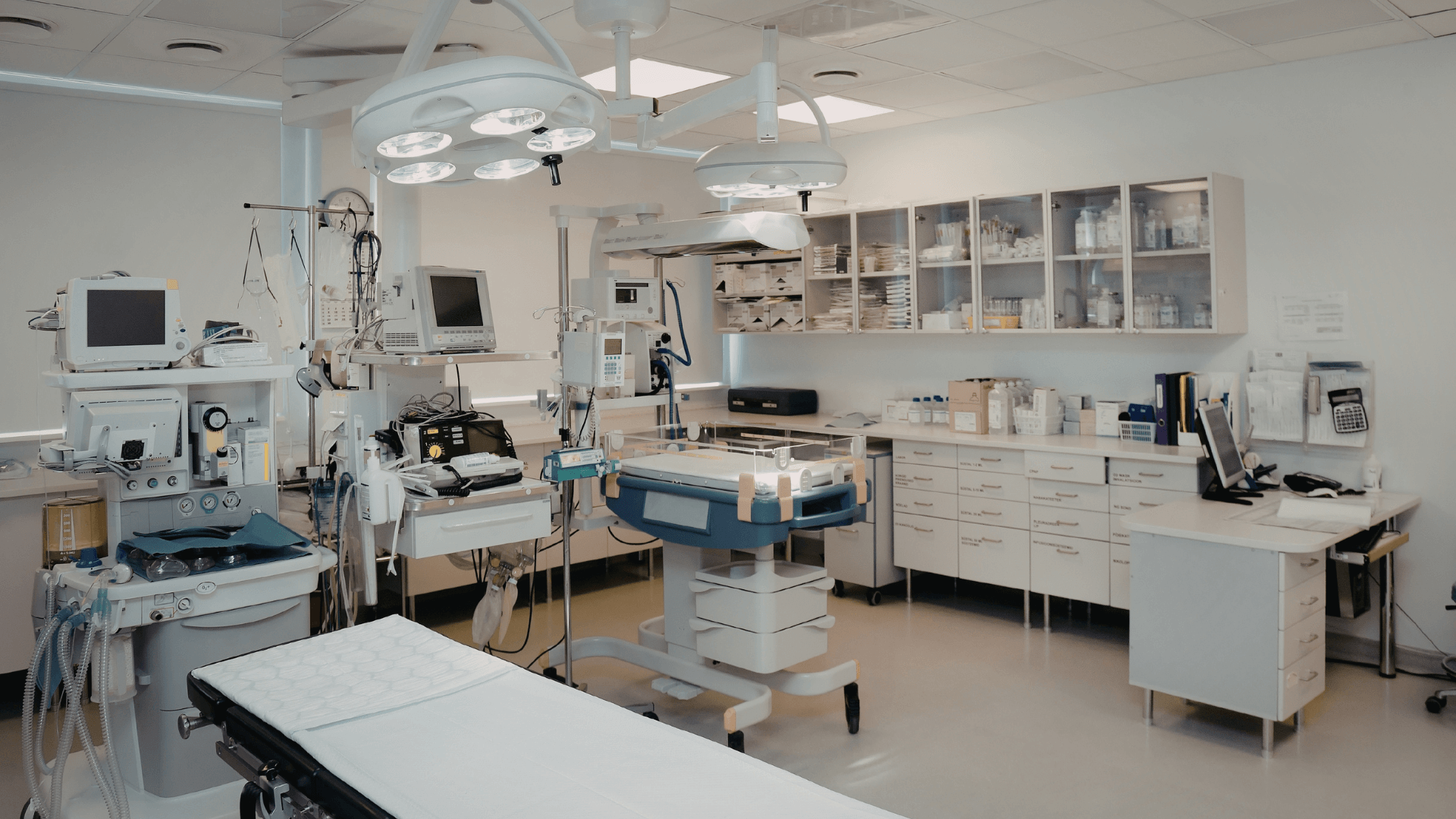
WHY HEALTH INSURANCE & TPA TRANSFORMATION CAN’T WAIT
The healthcare financing industry is under unprecedented pressure — rising medical inflation, complex regulatory demands, large claim volumes, member dissatisfaction, and increasing fraud risks.
At the same time:
Customers expect faster approvals and transparent communication
Hospitals demand quicker settlement cycles
Regulators require strong governance and compliance documentation
Fraud, waste & abuse (FWA) incidents continue to increase
Digital tools are reshaping claim management and utilization review
Data analytics is essential for pricing, risk modeling & cost control
Competition from digital insurtech players is rising
Health insurers and TPAs must operate with speed, accuracy, compliance, and digital visibility — and BGMC enables them to do exactly that.

BGMC’S TRANSFORMATION APPROACH — HEALTH INSURANCE & TPAS

Discover & Diagnose
A complete evaluation of claims workflows, medical review systems, customer service, provider networks, fraud controls, IT systems, workforce capability, and regulatory compliance.
We identify:
Delay drivers in claims & pre-authorization
Fraud & abuse indicators
Inconsistent medical review practices
Customer dissatisfaction factors
Weak provider governance & rate negotiation gaps
Digital readiness issues
Inefficiencies in documentation & approval loops
Output: A strategic roadmap with 10–14 priority improvements.
Design the Future Operating Model
We create a modern, efficient and compliant TPA/insurance operating model.
Includes:
Claims processing workflow redesign
Case management & utilization review models
Medical necessity review guidelines
Customer experience & call-center models
Provider network governance framework
SLA-based operations structure
Documentation & compliance architecture
Output: A scalable ecosystem for faster, compliant, customer-friendly operations.

Build & Pilot Using Digital, Lean & Compliance Systems
We develop and test optimized workflows in a controlled unit.
Capabilities include:
Digital claims triage & routing
Fraud detection models
Improved medical review procedures
Automated document management
Digital customer support tools
KPI dashboards (turnaround time, approval rates, costs)
Output: Measurable improvements in speed, accuracy, and customer confidence.

Scale & Industrialize Across the Organization
We expand the improved systems across all functions, regions, and portfolios.
We deploy:
Claims processing standards
Multi-provider network governance
Integrated case & disease management models
Real-time performance dashboards
Workforce training & medical reviewer upskilling
Output: Consistent, predictable performance across all business units.

Sustain & Upskill Your Workforce
Includes:
Claims examiner training
Fraud detection & risk management training
Customer service & communication skills
Healthcare coding (ICD/CPT) competency
Leadership development for supervisors & managers
Output: A skilled workforce capable of delivering high-quality service every day.

OUR HEALTH INSURANCE & TPA OFFERINGS
Operations Management for Claims, Approvals & Health Insurance Workflows
We streamline daily operations for faster claims, efficient preauthorizations, and consistent customer service.
Services include:
Claims workflow optimization
SLA-based process governance
Call-center & service process redesign
Backlog elimination
Daily performance routines
Example outcomes:
Faster resolution and lower operational burden.

Procurement & Vendor Management for Medical Networks
We optimize sourcing and management of service providers, hospitals, diagnostics, and partner vendors.
Services include:
Vendor governance frameworks
Hospital & lab contract optimization
Consumables & card issuance logistics
Provider auditing & rate benchmarking
Service delivery SLA enforcement
Example outcomes:
Better cost control and improved vendor reliability.

ISO & Regulatory Compliance for Health Insurers & TPAs
We help organizations meet national and international standards.
Services include:
ISO 9001, ISO 27001, ISO 22301 systems
Insurance regulatory compliance documentation
Risk management frameworks
Internal & external audit readiness
Business continuity planning
Example outcomes:
Stronger compliance posture and reduced regulatory risk.
Quality Management for Claims, Provider & Member Operations
We build systems for measurable and repeatable quality across the organization.
Services include:
Process audits & compliance checks
Quality metrics for claims & customer service
RCA & corrective action systems
SOP development & documentation control
Provider quality monitoring
Example outcomes:
Higher operational accuracy and service consistency.

Health, Safety & Confidentiality Management for Insurance & TPA Operations
We ensure safe, secure, and compliant environments for handling medical data.
Services include:
Data protection & confidentiality practices
Workplace safety governance
Stress & workload management systems
Secure document handling
Employee wellbeing programs
Example outcomes:
More secure operations & improved employee performance.

Project Management for System Upgrades, Network Expansion & Compliance Projects
We guide insurance and TPA organizations through major change initiatives.
Services include:
Claims system implementation PMO
Digital transformation & automation projects
Provider network expansion
Regulatory implementation programs
Cross-functional project governance
Example outcomes:
Faster adoption, fewer errors, and smooth change management.
Supply Chain for Medical Services, Cards, Devices & Support Operations
We optimize logistic flows for member cards, medical supplies, home-care support, and partner services.
Services include:
Medical service logistics coordination
Card issuance & delivery optimization
Home-care visit scheduling
Pharmacy & diagnostic partner flow management
Inventory control for consumables
Example outcomes:
Higher efficiency and reliable service delivery.
Digital Transformation for Health Insurance & TPAs
We modernize claims, approvals, customer support, and provider interactions using digital tools.
Services include:
AI-driven claims adjudication
Smart fraud detection systems
Customer portals & mobile apps
Field & provider engagement tools
Data analytics + BI dashboards
Example outcomes:
Reduced delays, improved accuracy, and stronger member satisfaction.

TECHNOLOGY STACK FOR HEALTH INSURANCE & TPAS
Example Use Cases & Outcomes
Reducing Claims Turnaround Time (TAT)
A TPA struggled with slow approvals and backlog.
Challenge: Manual workflows and inconsistent review.
Solution: Digital claims routing + SLA governance.
Outcome: TAT improved by 35% within 3 months.

Fraud Reduction in Provider Network
An insurer faced increasing fraudulent claims.
Challenge: Overbilling, upcoding, unnecessary procedures.
Solution: AI-based fraud detection + provider audits.
Outcome: Fraud losses reduced by 22%.

Improving Customer Experience
Members complained about slow responses and poor communication.
Challenge: Fragmented call center & unclear communication.
Solution: Omnichannel CX redesign + agent coaching.
Outcome: Complaint ratio decreased significantly.

Medical Cost Control
A health insurer experienced rising inpatient costs.
Challenge: Weak utilization review & LOS management.
Solution: Case management + discharge planning tools.
Outcome: Medical cost reduced by 14%.

Who We Serve
Industries
- Health Insurance Companies
- Third-Party Administrators (TPAs) Managed Care Organizations
- Corporate Health Benefit Managers Hospitals & Provider Networks
- Insurtech Firms Government Healthcare Buyers
- Employer Health Plans
Functions
- Claims
- Underwriting
- Medical Review
- Provider Management
- Customer Service
- Supply Chain
- IT
- Compliance
- Leadership
Regions
Frequently Asked Questions
1. Can BGMC help reduce claims turnaround time?
2. Do you help with fraud detection and risk control?
3. Can BGMC support ISO and regulatory compliance?
4. Do you assist with digital transformation?
5. Do you offer staff training in claims, medical review, and customer service?
Ready to Transform Your Manufacturing Operations?
Let’s discuss how BGMC Group can help transform your operations and drive measurable results.
Connect with our experts today to explore customized industrial and business solutions designed for your success.
We work with ambitious leaders who want to define the future, not hide from it. Together, we achieve extraordinary outcomes.
